Gut–Brain Axis & Enteric Nervous System (ENS)
Peripheral neural–immune interface — microbial metabolites, vagal signalling, immune–metabolic integration.
Overview
The gut microbiome represents a critical biological target in the BRAIN Diet, focusing on supporting beneficial gut bacteria and optimizing the gut-brain axis communication. A growing body of evidence suggests that modulating the gut microbiome can positively influence brain health and overall health. The gut is central in producing neurotransmitters, reducing systemic inflammation and enhancing gut-brain axis communication with fibre and fermented foods playing a central role in all of those processes (paper.txt, line 496).
Recipes
Therapeutic Areas
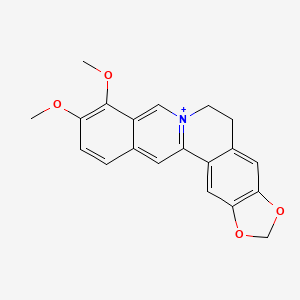
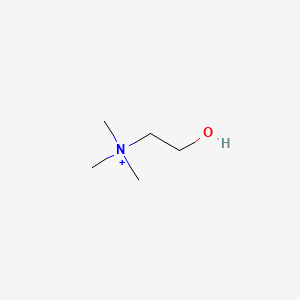
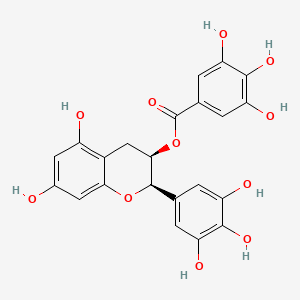
Substances
Foods supporting SCFA production
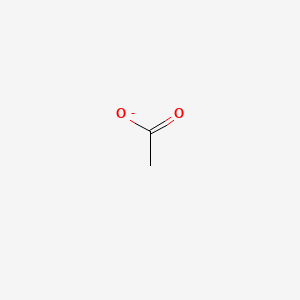
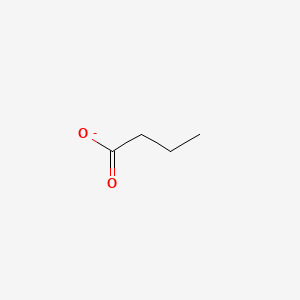
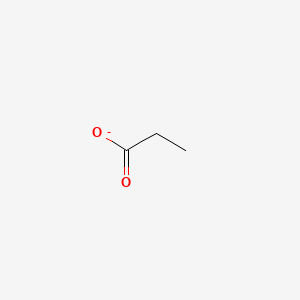
Foods that support production of short-chain fatty acids (butyrate, propionate, acetate) or provide them in the diet help populate the Biological Target Matrix and therapeutic-area matrices. Use the lists below to isolate foods by SCFA.
All foods supporting SCFAs
Foods associated with butyrate (resistant starch, inulin, dietary sources)
Foods associated with propionate
Foods associated with acetate
Biological Implications
The gut microbiome's two dominant bacterial phyla are Firmicutes and Bacteroidetes, and their relative abundance (the Firmicutes:Bacteroidetes (F/B) ratio) is often considered a broad indicator of gut "balance" or dysbiosis. Studies have shown how by increasing the diversity of taxa can increase the possibilities for individuals to produce certain health beneficial metabolites such as Urolithin A, or increase omega 3 metabolism and reduce downstream harmful gut metabolites (paper.txt, line 497).
Studies have shown conflicting results in categorising microbiota of ADHD subjects and in general the taxonomy is still evolving. Some studies noted reduced levels of beneficial bacteria such as Faecalibacterium prausnitzii and Bifidobacterium, but conversely other studies found that individuals with ADHD had slightly increased Bifidobacterium. The key is really dealing with gut bacteria at the strain level, as different species within the same genus can have different functional impacts (paper.txt, line 499).
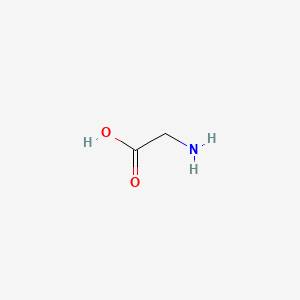
The gut-brain connection may also play a significant role in the etiology of ADHD. Gut health influences the production of neurotransmitters and their precursors, including serotonin, gamma-aminobutyric acid (GABA), and dopamine. While gut-derived neurotransmitters are unlikely to cross the blood–brain barrier (BBB), their precursors, such as tryptophan and tyrosine, do, enabling local synthesis in the brain (paper.txt, line 502).
In addition, gut–brain signaling occurs via the vagus nerve, which transmits microbial and neurochemical cues to influence mood and motivation. Vagal stimulation has demonstrated clinical benefits in depression, epilepsy, and inflammation while preclinical work shows that gut microbes such as Lactobacillus can alter brain GABA receptor expression through vagal pathways (paper.txt, line 503).
The gut barrier is the dynamic interface between the microbiome, immune system, and brain. Its integrity is critical: when the barrier weakens, bacterial fragments such as lipopolysaccharide (LPS, a bacterial endotoxin) and dietary antigens enter circulation, sustaining chronic low-grade inflammation and altering neurotransmitter metabolism. These processes are strongly correlated with poor cognitive function, fatigue, mood instability, and ADHD symptom severity (paper.txt, line 505).
The barrier is organized into four interdependent layers, each with distinct vulnerabilities that can compromise brain health: microbiota layer (weakened by loss of fibre and polyphenols; reduced SCFA production removes protection against pathogens), mucus layer (eroded by low plant diversity and ultra-processed foods), epithelial layer (disrupted by nutrient deficiencies, alcohol, NSAIDs, and chronic stress, increasing permeability), and immune layer (dysregulated by omega-3 deficiency and low vitamin A) (paper.txt, lines 507-510).
When these weaknesses converge, lipopolysaccharide (LPS) crosses into the bloodstream, fueling systemic inflammation, impairing insulin sensitivity, and that inflammation has also been linked to disrupting dopamine and serotonin pathways and causing depression. Metabolic endotoxemia (ME), defined as chronically elevated circulating lipopolysaccharide (LPS), is very common, with estimates of up to one-third of adults in Western populations, particularly those with obesity or high-fat, low-fibre diets. Even modest elevations in LPS can sustain low-grade inflammation, impair insulin sensitivity, and promote neuroinflammatory cascades that compromise dopamine signaling and cognitive resilience. Similarly, small intestinal bacterial overgrowth (SIBO) impairs absorption of vitamin B12, iron, and tryptophan, depriving the brain of essential neurotransmitter precursors (paper.txt, line 511).
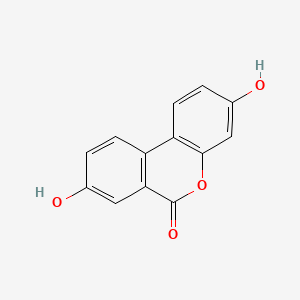
Interventions such as prebiotics, probiotics, high-fibre diets, and fermented foods, collectively referred to in emerging research as psychobiotics, have been associated with changes in attentional vigilance and mood regulation with galacto-oligosaccharides (GOS) being linked to reduced anxiety and cortisol. These effects are thought to be, in the main, mediated through increased production of short-chain fatty acids (SCFAs) like butyrate, which support intestinal barrier integrity, regulate immune responses, antioxidant activity, and promote the synthesis of key neurotransmitters such as dopamine and serotonin (paper.txt, line 516).
Diets rich in probiotics, prebiotics, and fibre (which help produce short-chain fatty acids like butyrate, propionate and lactate) can enhance gut health. Furthermore, a decreased microbial diversity (alpha diversity) has also been reported in ADHD and may contribute to 'leaky gut' syndrome and contribute to the low-grade systemic inflammation reported in ADHD (paper.txt, line 521).
Butyrate has anti-inflammatory effects, potentially reducing neuroinflammation associated with ADHD. Butyrate supports mitochondrial function, enhancing brain energy metabolism, which may help with cognitive impairments seen in ADHD while also aiding in reducing cholesterol and neuroinflammation (paper.txt, lines 525-526).
Propionate research suggests that increased propionate levels could help reduce neuroinflammation and enhance cognitive function while protecting the blood-brain barrier and stimulate the secretion of norepinephrine, possibly benefiting ADHD symptoms like attention and focus (paper.txt, line 527).
A lowered abundance of Bifidobacterium longum in infancy has been associated with increased risk of developing ADHD and Asperger syndrome in childhood; the same study also showed early administration of Lactobacillus rhamnosus GG may reduce the risk of ADHD and AS, however due to the small study size, such findings are best interpreted as hypothesis-generating, highlighting a potentially critical early-life window for microbiome modulation rather than providing definitive evidence of prevention (paper.txt, line 529).
References
- A growing body of evidence suggests that modulating the gut microbiome can positively influence brain health and overall health. The gut is central in producing neurotransmitters, reducing systemic inflammation and enhancing gut-brain axis communication with fibre and fermented foods playing a central role Wastyk et al. 2021
- Increasing the diversity of taxa can increase the possibilities for individuals to produce certain health beneficial metabolites such as Urolithin A, or increase omega 3 metabolism and reduce downstream harmful gut metabolites Schleupner and Carmichael 2022
- Some studies noted reduced levels of beneficial bacteria such as Faecalibacterium prausnitzii and Bifidobacterium in ADHD subjects Wang et al. 2024
- Conversely, other studies found that individuals with ADHD had slightly increased Bifidobacterium Aarts et al. 2017
- The gut-brain connection may also play a significant role in the etiology of ADHD Jiang et al. 2018
- Gut–brain signaling occurs via the vagus nerve, which transmits microbial and neurochemical cues to influence mood and motivation. Vagal stimulation has demonstrated clinical benefits in depression, epilepsy, and inflammation Austelle et al. 2022
- Gut microbes such as Lactobacillus can alter brain GABA receptor expression through vagal pathways Bravo et al. 2011
- A decreased microbial diversity (alpha diversity) has also been reported in ADHD Prehn-Kristensen et al. 2018
- Interventions such as prebiotics, probiotics, high-fibre diets, and fermented foods, collectively referred to as psychobiotics, have been associated with changes in attentional vigilance and mood regulation Schmidt et al. 2015
- Galacto-oligosaccharides (GOS) being linked to reduced anxiety and cortisol Johnstone et al. 2021
- Short-chain fatty acids (SCFAs) like butyrate support intestinal barrier integrity, regulate immune responses, antioxidant activity, and promote the synthesis of key neurotransmitters such as dopamine and serotonin Silva et al. 2020
- Butyrate supports mitochondrial function, enhancing brain energy metabolism, which may help with cognitive impairments seen in ADHD Rose et al. 2018
- Butyrate aids in reducing cholesterol and neuroinflammation Cavaliere et al. 2022
- Increased propionate levels could help reduce neuroinflammation and enhance cognitive function while protecting the blood-brain barrier Grüter et al. 2023
- Propionate can stimulate the secretion of norepinephrine, possibly benefiting ADHD symptoms like attention and focus Hoyles et al. 2018
- A lowered abundance of Bifidobacterium longum in infancy has been associated with increased risk of developing ADHD and Asperger syndrome in childhood Pärtty et al. 2015