Insulin Response
Overview
Insulin response optimization is a critical biological target in the BRAIN Diet, focusing on maintaining stable blood glucose levels and improving insulin sensitivity to support cognitive function and reduce inflammation. ADHD and some other neuropsychiatric conditions (e.g., ASD, Bipolar and MDD) may represent a cluster of disorders influenced by brain-specific insulin dysregulation. Insulin plays a central role in brain function, modulating neurotransmitter balance, synaptic plasticity, and cellular energy metabolism. Beyond standard fasting glucose measures, continuous glucose monitoring (CGMs) offers novel insights into postprandial spikes and glycemic variability (paper.txt, line 780).
Recipes
Therapeutic Areas
Substances
Biological Implications
Because the brain has limited capacity to store energy, maintaining a steady supply of glucose is essential for optimal cognitive function, unless a ketogenic dietary pattern is being followed, and risks have to be carefully assessed (paper.txt, line 489).
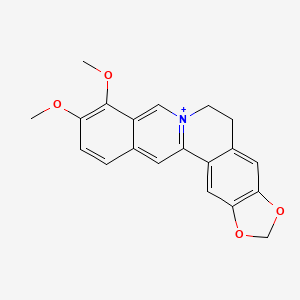
ADHD and some other neuropsychiatric conditions (e.g., ASD, Bipolar and MDD) may represent a cluster of disorders influenced by brain-specific insulin dysregulation. Insulin plays a central role in brain function, modulating neurotransmitter balance, synaptic plasticity, and cellular energy metabolism. Altered glucose uptake has been observed in ADHD, with PET studies showing reduced metabolism in prefrontal and striatal regions (paper.txt, lines 780, 782).
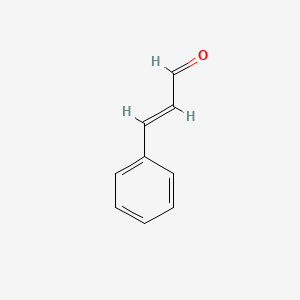
A classic milestone study demonstrated that apple juice induces a substantially greater postprandial insulin spike and lower satiety compared to either apple purée or the intact fruit, underscoring the role of food structure in metabolic responses. More recent work has extended these observations to the brain, linking attenuated glycemic excursions from intact food matrices to preserved brain insulin sensitivity, improved dopaminergic regulation, and more balanced reward processing. Preserving natural food structure (e.g., an apple vs. processed forms) blunts post-prandial glycemic excursions, supports brain insulin sensitivity, and stabilizes dopamine–insulin coupling, mechanisms that may help regulate motivation and reduce impulsive behaviors (paper.txt, lines 177, 180).
Managing glycemic variability stabilizes dopamine–insulin coupling and cognitive performance. Glycemic stabilization is expected to exert downstream effects on emotional regulation through modulation of HPA axis activity, limbic signalling, and neurotransmitter systems (paper.txt, line 335).
While epidemiological studies suggest the prevalence of metabolic syndrome in adults with ADHD (~10.8% under 60) does not exceed general population norms, there is substantial evidence of mechanistic overlap. ADHD often co-occurs with obesity, insulin resistance, and dysglycemia with shared pathophysiological pathways including dopaminergic reward circuit impairment, HPA-axis disturbances, chronic low-grade inflammation, and oxidative stress. These pathways create reciprocal vulnerability: metabolic dysfunction amplifies ADHD symptoms, and ADHD behaviors and lifestyles (poor diet, stress reactivity, irregular sleep) worsen metabolic risk and ADHD symptoms (paper.txt, line 777).
Prenatal exposures further highlight the metabolic link. Maternal diabetes is associated with significantly increased ADHD risk in offspring, with meta-analyses estimating a 44% increase overall and higher risk for pre-existing diabetes compared to gestational diabetes. Chronic maternal hyperglycemia and inflammation during neurodevelopment likely underpin this effect (paper.txt, line 778).
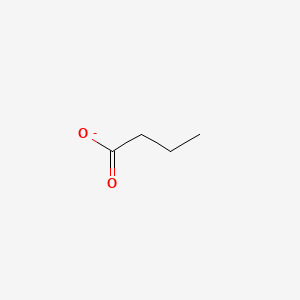
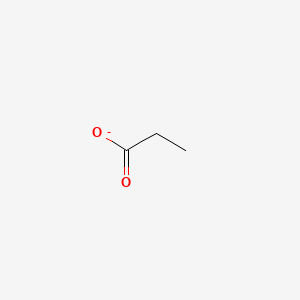
Beyond circadian disruption, chronic consumption of added sugars, particularly fructose-containing sweeteners such as sucrose and high-fructose corn syrup, exerts unique metabolic stress. Randomised trials show sugar-sweetened beverage intake drives dose-dependent increases in visceral adiposity, dyslipidaemia, and insulin resistance, even independent of weight gain. For ADHD populations already vulnerable to glucose variability and reward-driven eating, high sugar intake may compound both metabolic and neurocognitive dysregulation. As discussed above, sugars delivered within whole foods such as fruit or dairy are buffered by fibre, polyphenols, and micronutrients, producing more stable glycaemic responses (paper.txt, line 784).
Adipose tissue further links metabolic health with brain function. Dysfunctional visceral adipose depots release pro-inflammatory cytokines that cross the blood–brain barrier and disrupt neurotransmission. Nuclear receptors such as PPAR-α and PPAR-γ, which regulate fatty acid oxidation, insulin sensitivity, and adipokine release, are central to this process. Omega-3 fatty acids act as partial agonists of PPARs, promoting mitochondrial efficiency and anti-inflammatory signaling. Their activation shifts adipose tissue toward a metabolically protective phenotype, with downstream benefits for neuroimmune stability (paper.txt, line 788).
The Green Mediterranean Diet study produced greater visceral adipose tissue (VAT) loss than MED or control (≈ −14.1% vs −6.0% vs −4.2%); VAT loss tracked with higher total plasma polyphenols and with the microbiome-derived markers urolithin A (via ellagitannins: walnuts/pomegranate) and hippuric acid from green tea catechins. Parallel analyses showed MED/green-MED attenuated brain atrophy by ~50%, with glycemic control contributing to the neuroprotective signal, consistent with a polyphenol–fibre–microbiome synergy improving metabolic and brain aging phenotypes (paper.txt, line 790).
Beyond adipose-derived cytokines, microbial lipopolysaccharides (LPS) can enter systemic circulation through increased gut permeability, amplifying low-grade inflammation and impairing insulin sensitivity. Dietary polyphenols, prebiotic fibres, and lactobacilli strains have been shown to reduce LPS translocation and neutralize its inflammatory signaling, underscoring the microbiome's role in HPA–ANS stability (paper.txt, line 789).
Aligning nutrient intake with circadian and activity rhythms represents the science of chrono-nutrition which if followed can represent lower metabolic stress if we eat in line with our biological clock. Failing to do so is associated with increased adiposity, T2DM, and cardiometabolic risk factors. Chrono-nutrition is based on three different dimensions of eating behavior, including timing, frequency, and regularity. In ADHD, where appetite suppression from medications, irregular eating, and sleep disruption are common, timing nutrients appropriately may optimize energy regulation, neurotransmitter production and cognitive function (paper.txt, lines 823-824).
Earlier and more consistent eating windows are associated with improved weight and glycaemic outcomes. These benefits are partly explained by circadian biology in that adipose tissue insulin sensitivity is up to 54% higher at noon than at midnight (paper.txt, line 843).
Thiamine (B1) is essential for mitochondrial glucose metabolism in the brain leading to ATP production (paper.txt, line 710).
References
- ADHD and some other neuropsychiatric conditions (e.g., ASD, Bipolar and MDD) may represent a cluster of disorders influenced by brain-specific insulin dysregulation Fanelli et al. 2022
- Because the brain has limited capacity to store energy, maintaining a steady supply of glucose is essential for optimal cognitive function, unless a ketogenic dietary pattern is being followed, and risks have to be carefully assessed Crosby et al. 2021
- Altered glucose uptake has been observed in ADHD, with PET studies showing reduced metabolism in prefrontal and striatal regions Zametkin et al. 1990
- A classic milestone study demonstrated that apple juice induces a substantially greater postprandial insulin spike and lower satiety compared to either apple purée or the intact fruit, underscoring the role of food structure in metabolic responses Haber et al. 1977
- More recent work has extended these observations to the brain, linking attenuated glycemic excursions from intact food matrices to preserved brain insulin sensitivity, improved dopaminergic regulation, and more balanced reward processing Gruber et al. 2023
- The BRAIN Diet uses nutrient-timed meals to support dopamine–insulin coupling through dopamine precursors and anti-inflammatory nutrients to reduce DMN dysregulation Marsland et al. 2017
- Maternal diabetes is associated with significantly increased ADHD risk in offspring, with meta-analyses estimating a 44% increase overall Guo et al. 2020
- Higher risk for pre-existing diabetes compared to gestational diabetes Damtie et al. 2025
- Chronic maternal hyperglycemia and inflammation during neurodevelopment likely underpin this effect Wimberley et al. 2024
- Chronic consumption of added sugars, particularly fructose-containing sweeteners such as sucrose and high-fructose corn syrup, exerts unique metabolic stress Stanhope 2016
- Randomised trials show sugar-sweetened beverage intake drives dose-dependent increases in visceral adiposity, dyslipidaemia, and insulin resistance, even independent of weight gain Sampasa-Kanyinga et al. 2018
- Adipose tissue insulin sensitivity is up to 54% higher at noon than at midnight Poggiogalle et al. 2018